Adult Cleft Rhinoplasty & Cleft Lip Revision in Dallas, Texas
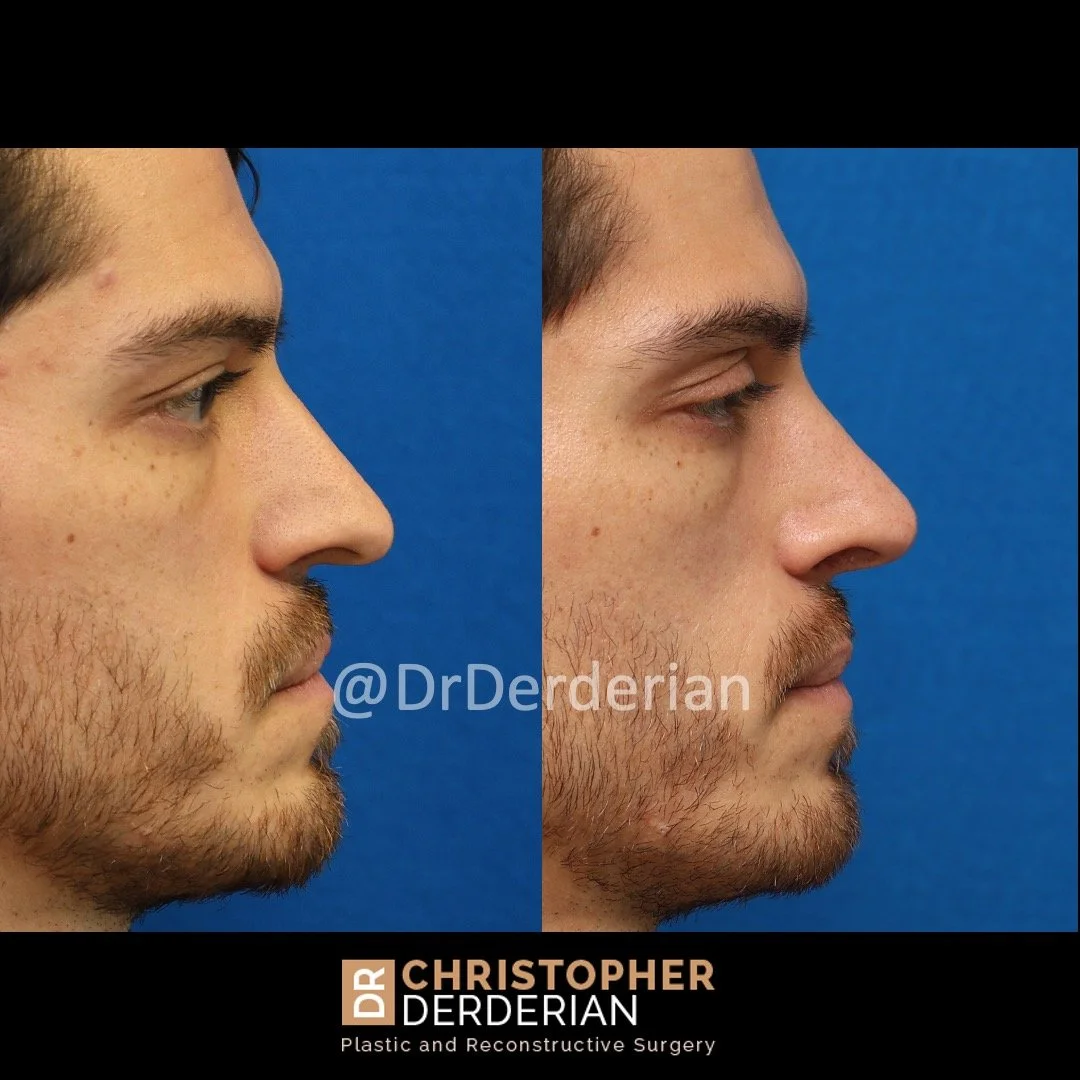
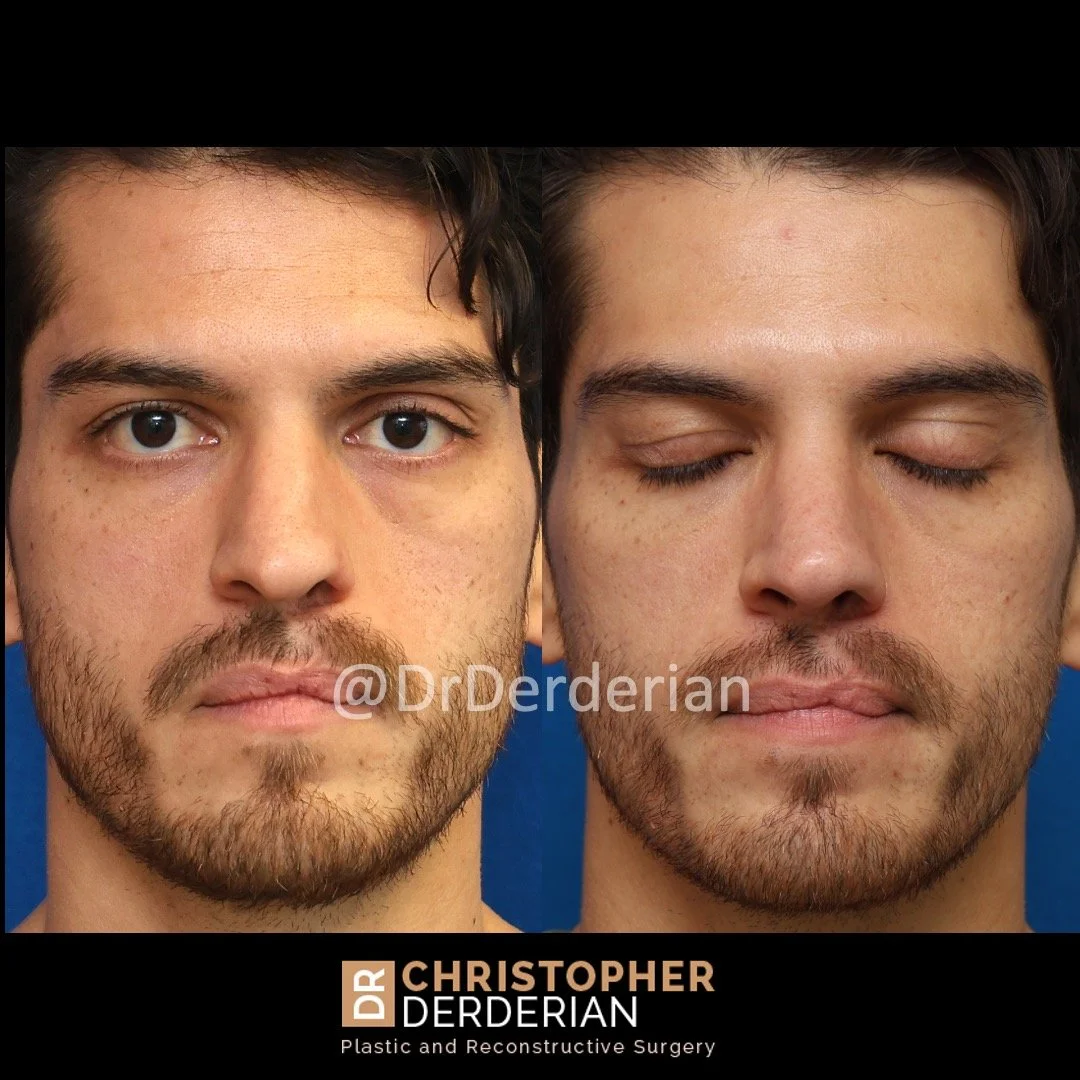
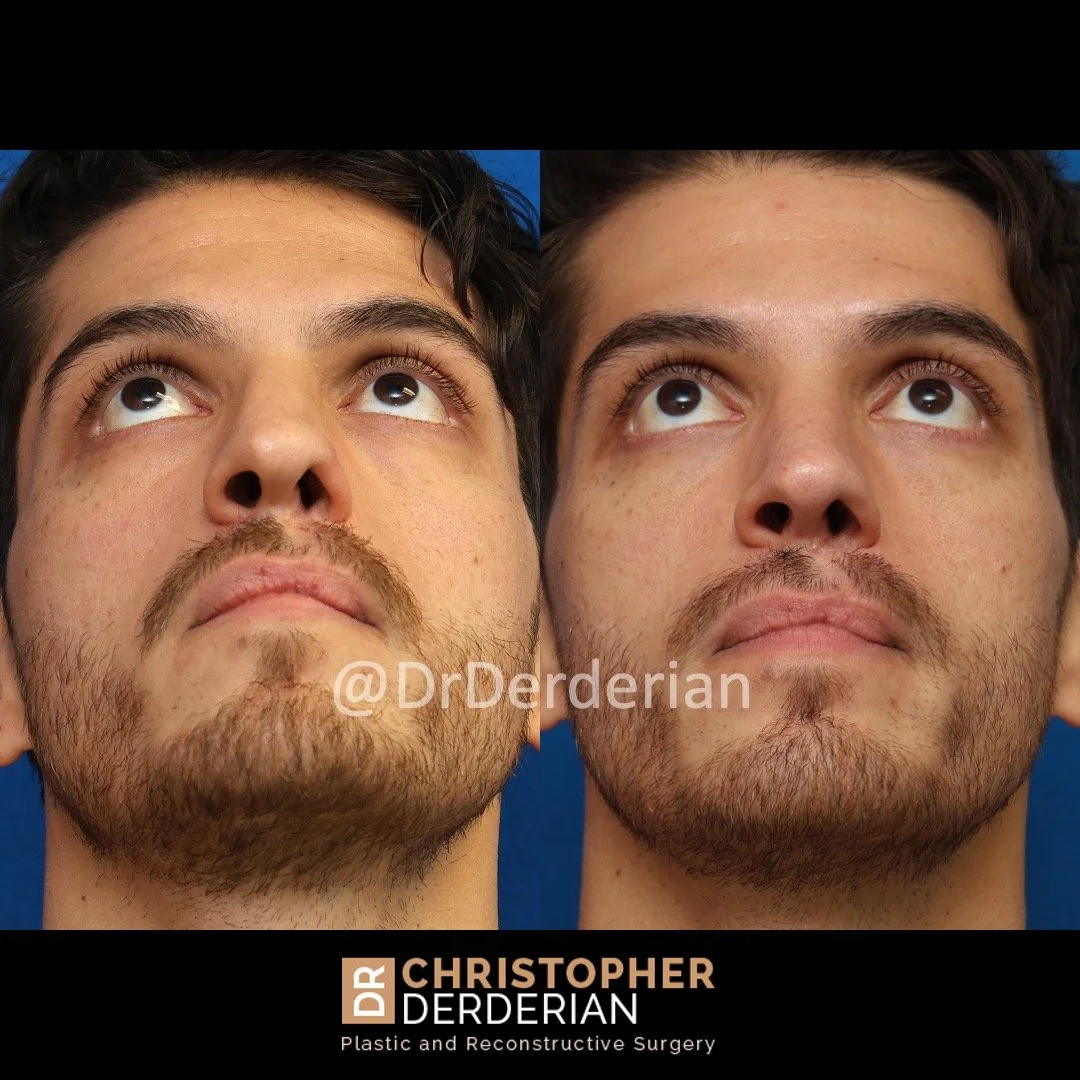
A cleft lip revision is a surgery performed to improve the appearance of the scar from cleft lip repair, to improve the symmetry of the upper lip and/or to improve deficient bulk in the upper lip that remains after cleft lip repair. Cleft rhinoplasty is a surgery performed to correct the stigmatizing appearance of the nose caused by cleft lip. Cleft rhinoplasty commonly involves making the nostrils symmetric, straightening a crooked nose and improving the definition, symmetry and projection of the nasal tip.
Over the past ten years, I have cared for more and more adult patients who were born with cleft lip and remain unhappy about the appearance of their lip and nose, leaving them self-conscious about their appearance. Anyone with concerns about the appearance of their lip or nose due to cleft lip should know that they are not alone. Cleft lip is the most common congenital facial difference. Even though you may have been told that you have had all of the surgeries that you needed as a child, and you may have had good relationships with your surgeons, you may still be unhappy with your appearance. Your concerns are valid.
The techniques for performing cleft lip revision and cleft rhinoplasty do not differ much between teenagers and adults. Unfortunately, adults with concerns about the appearance of their lip and nose often feel that they don’t have a good option for them to go to for care. Since all of the treatment for cleft care is supposed to be “finished” before adulthood, there are few places that focus on caring for adult patients with concerns about their appearance related to cleft lip and palate. For adults, it may feel strange and uncomfortable to get a consultation for surgery at a children’s hospital where most surgeons performing procedures related to cleft lip and palate practice. As a result, adults with appearance concerns related to their cleft lip frequently turn to plastic surgeons in the community who only see adult patients. While these surgeons may exclusively care for adults, they may have little or no experience in cleft lip surgery or cleft rhinoplasty. Unfortunately, the surgical techniques that are commonly used for cosmetic rhinoplasty are not effective in the treatment of the cleft lip nasal deformity. This leaves patients frustrated from going through the pain of surgery and recovery and the cost of surgery with disappointing results. I hear this story often.
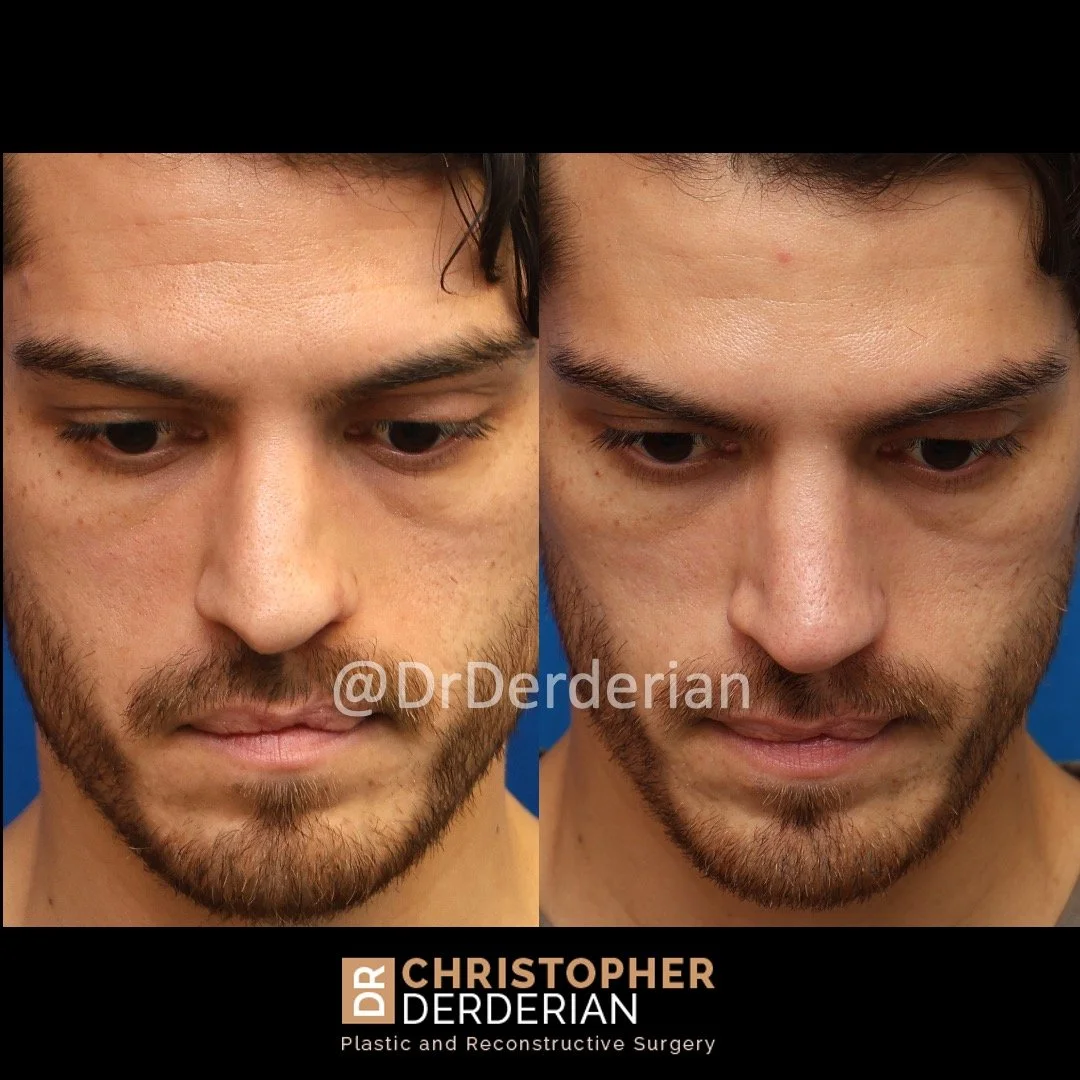
Cleft rhinoplasty is widely considered to be the most difficult rhinoplasty to achieve consistently good results. There are few procedures in plastic surgery with as many nuances as cleft rhinoplasty or cleft lip revision. It is critical to find a plastic surgeon with expertise in cleft lip revision and cleft rhinoplasty to achieve an aesthetically pleasing and natural appearance after surgery. Likewise, the breathing concerns related to the cleft nasal deformity are considerable, and experience is needed to achieve a lasting improvement in breathing. I share some before and after example photos of my patients on this page and in my cleft rhinoplasty and cleft lip revision photo gallery to demonstrate the improvement that can be achieved in a variety of cases.
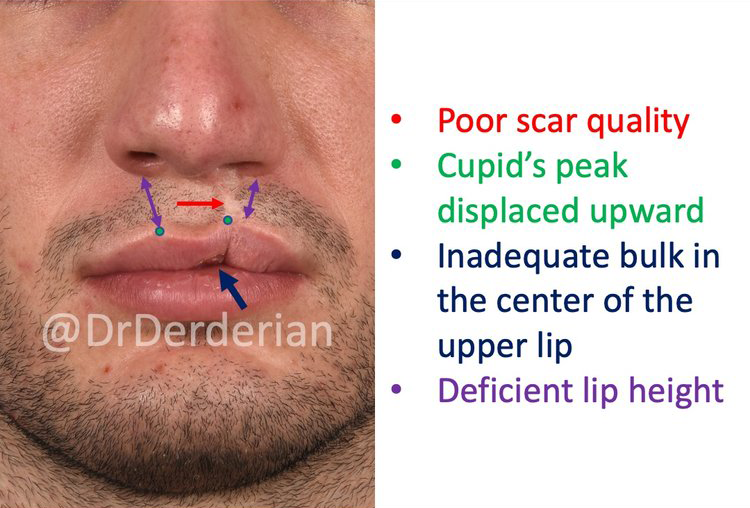
Common reasons why Patients Seek Cleft Lip Revision include:
An uneven appearance of the upper lip
Poor scar quality from the cleft lip repair
A pulled up appearance of the upper lip at the cleft site
Inadequate bulk in the central portion of the lip (“Whistle Deformity”)
Uneven height of the upper lipIncrease Projection of the Nasal Tip
Disruption of the white roll
Common reasons why patients seek Cleft Rhinoplasty include:
Make the nose look more symmetric overall
Make the nostril rims look more symmetric
Improve definition of a nasal tip that is uneven and/or wide
Increase Projection of the Nasal Tip
Straighten a crooked nose
Narrow a wide nostril base
Improve the profile by lengthening a short nose
Improve the profile by removing bumps or dips in the dorsum (bridge) of the nose
Change the size and shape of the nose to improve facial balance
Improve breathing through the nose
-
It is typically best to wait at least 1 year from the time of the most recent nasal surgery to seek consultation for cleft rhinoplasty. This provides time for swelling to fully resolve and gives the healing process time to complete and allow the skin and soft tissue to soften. The best candidates for cleft rhinoplasty are healthy, do not smoke (or are willing to quit smoking) and have realistic goals for what can be achieved from surgery.
-
Dr. Derderian uses an open approach to cleft rhinoplasty because the open approach allows direct visualization of the nasal cartilages. Open rhinoplasty requires a small incision in the columella (the skin between the nostrils) with the remaining incisions made inside the nose. Through this approach the skin of the nose is elevated off of the underlying cartilage and bone that allows all surgical maneuvers to be performed under direct visualization. This incision typically heals with an imperceivable scar.
The duration of surgery varies from patient-to-patient depending on if the lip is being revised and the scope of the lip revision. Typically the procedure takes about 5 hours. Depending on the strength and position of the nasal cartilages and bones and the goals of surgery, a variety of maneuvers are used to reshape the nose and improve breathing. Graft material is needed in every cleft rhinoplasty to change the shape of the nose. Cartilage from the nasal septum is the easiest site to get cartilage grafts from, and the nasal septum usually requires straightening during the procedure. However, the a large amount of graft material is needed to successfully reshape the nose in cleft rhinoplasty. The skin and soft tissues of the nose are very scarred and stiff and strong cartilage is needed to achieve a durable result. Rib cartilage is the only other source for cartilage grafts that has the strength needed in cleftt rhinoplasty. Dr. Derderian frequently uses an alternative source of rib cartilage harvested from organ donors (MTF Profile Costal Cartilage) that has been treated to remove all immune markers that prevents rejection of the graft. Using donor cartilage avoids additional pain and recovery for the patient.
After the desired changes in shape are achieved the nose is closed with fine stitches. At the end of surgery soft splints may be placed inside your nose to support the nasal septum. Soft splints are frequently used on the outside of the nose also to help shape the skin. Tapes and a splint are placed over the nasal bridge to support and protect the nose for 7 days. After recovering from anesthesia you will be taken home the same day as surgery by the family or friends who bring you to the hospital.
-
Minimal activity is recommended for the week after surgery. Most patients take at least one week off from work or school. Oral pain medication is used for 2-3 days. The nasal splints and sutures are removed 7 days after surgery. No heavy lifting or activity that gets the heart rate elevated is allowed for 2weeks. After 2 weeks a gradual resumption of normal cardiovascular exercise and non contact sports may be resumed. No restrictions on activity after 6 weeks.
The majority of swelling subsides within a few weeks after surgery. Even with significant swelling present one week after surgery, the improved appearance of the lip and nose is easy to appreciate. At 1 week after surgery you will feel swollen, but patients feel comfortable being out in public and socializing. For the first 3-4 weeks after surgery it is difficult to breathe through the nose because of swelling. By 6 weeks after surgery, there is minimal residual swelling, breathing should be improved and the improved symmetry and proportions of the lip and nose will be appreciable. It actually takes 1 year for the swelling to completely resolve. During this time, your nose will essentially look the same but, if you carefully compare photos of your nose at 6 weeks, 6 months and 1 year after surgery, you will notice subtle changes in the nasal tip with a more refined appearance as the trace residual swelling resolves.
-
It is critical to have an experienced surgeon perform your cleft rhinoplasty. During his plastic surgery training Dr. Derderian had extensive training in cleft rhinoplasty at New York University with Dr. Court Cutting, a world-renowned authority in cleft surgery. After completing his residency, Dr. Derderian did a fellowship in craniofacial surgery at the University of Pennsylvania and Children’s Hospital of Philadelphia where he received additional experience performing cleft rhinoplasty. Dr. Derderian is board certified by the American Board of Plastic Surgery and is a member of the Cleft and Craniofacial Team at Children’s Health Dallas. Cleft rhinoplasty is a focus of Dr. Derderian’s practice and clinical research. He frequently performs cleft rhinoplasty in both his pediatric and adult practices. Dr. Derderian’s clinical research focuses on nasal growth in patients with cleft lip and palate studying the aesthetic and functional outcomes from cleft rhinoplasty. He has been invited yearly as an instructor at the world renowned Dallas Rhinoplasty Symposium since arriving in Dallas in 2011, and he has been selected for D Magazine best doctors edition annually since 2015.